Amniotic band syndrome
(1) Femicare, Center of prenatal ultrasonographic diagnostics, Martin, Slovakia; (2) Centro Médico Recoletas, Valladolid, Spain
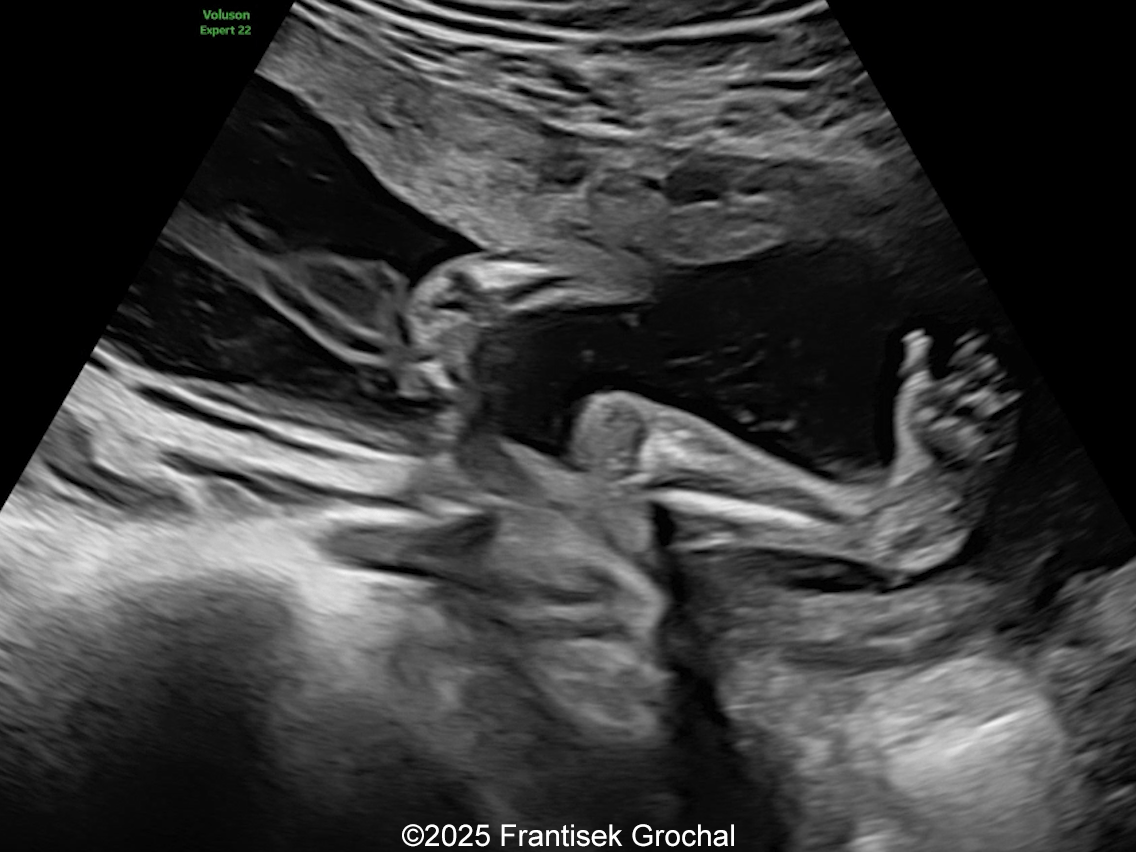
A 30-year-old G2P1, with an unremarkable history, presented to our office in the 21st week of her pregnancy for a routine second-trimester screening. Our examination revealed the following findings:

View the Answer Hide the Answer
Answer
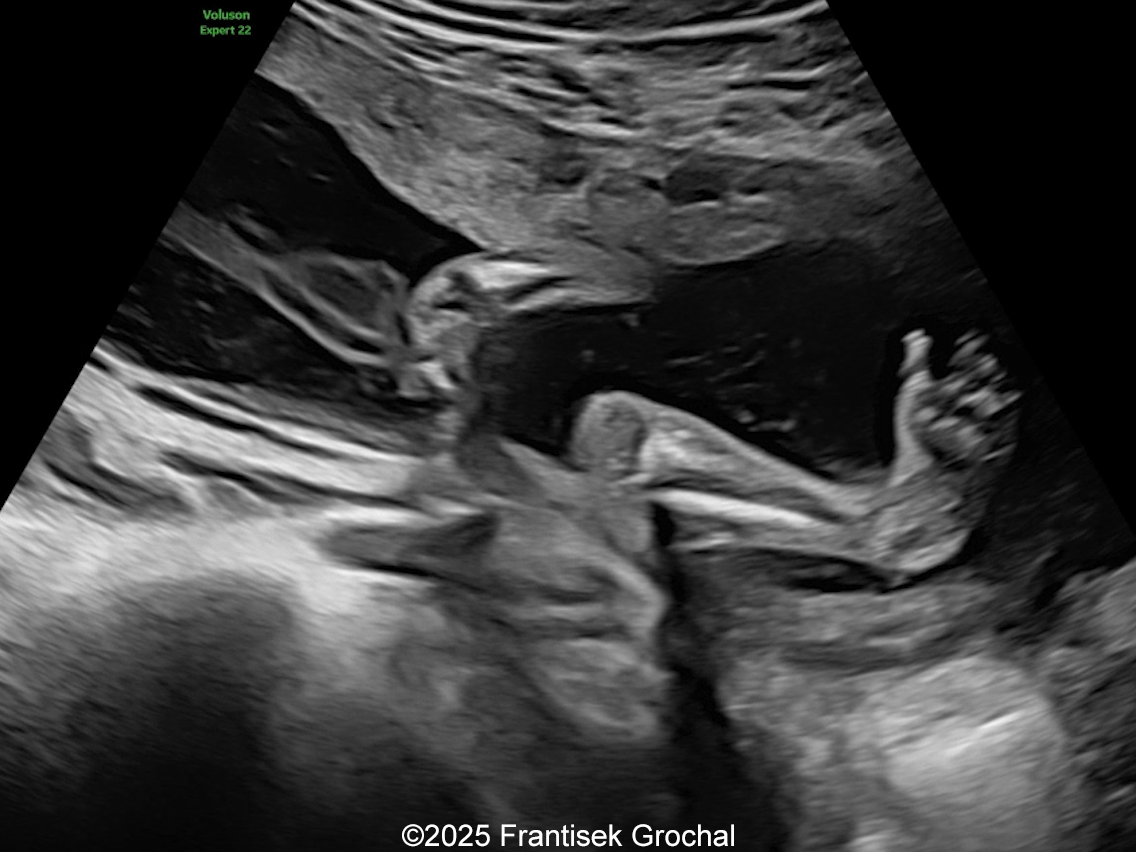
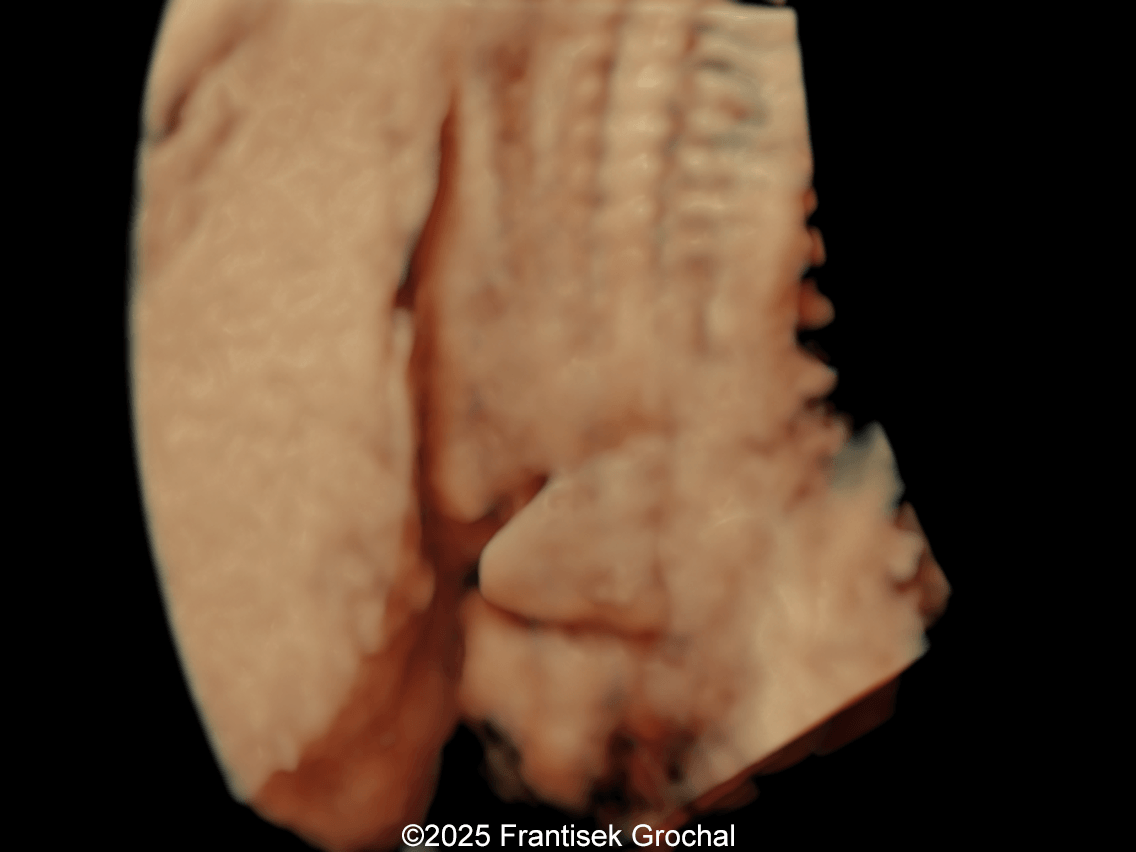
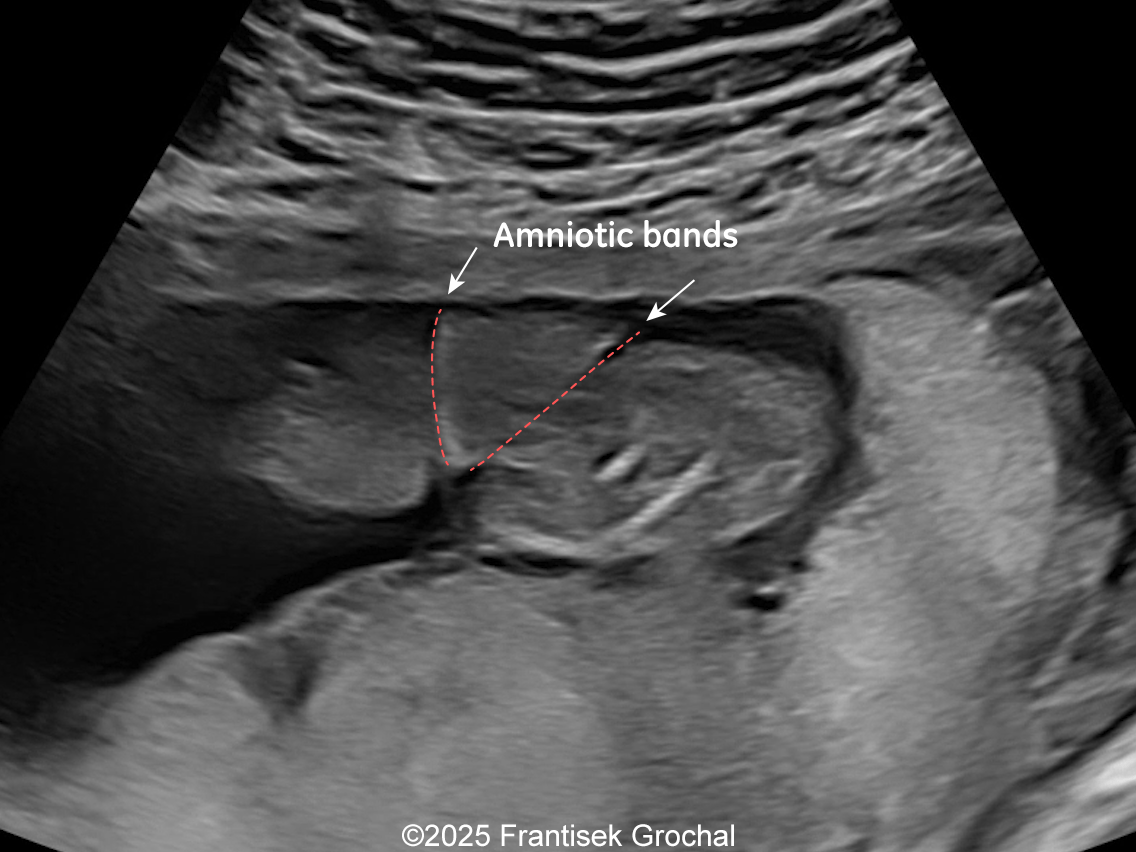
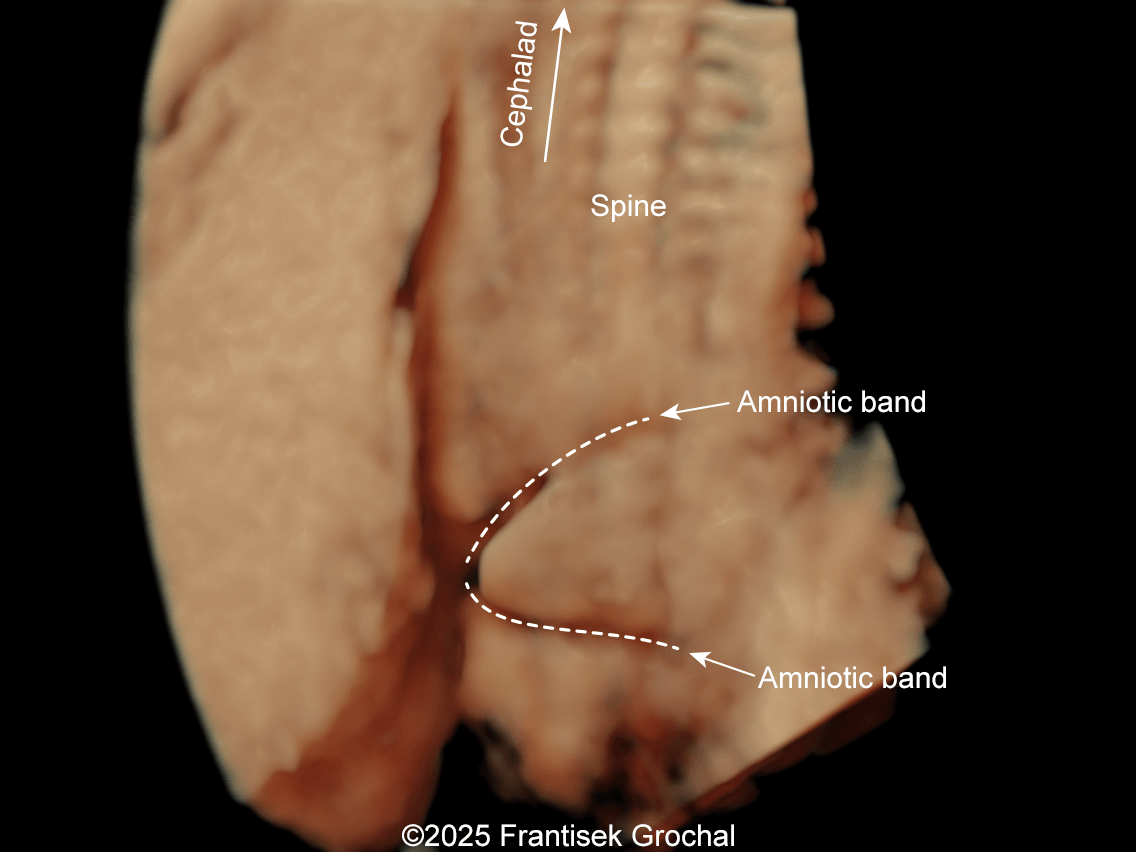
We present a case of Amniotic Band Sequence seen in 21st week of pregnancy. The fetus showed the following findings:
- Bilateral club feet
- Constriction of the right thigh by the amniotic band
- Constriction of fetal torso by two strips of amniotic band
The mother was sent to a specialized perinatology center for a planned minimally invasive amniotic band resection. Unfortunately, one week later, just before the procedure, spontaneous demise of the fetus occurred. Amniotic band sequence was confirmed.

Discussion
Amniotic band sequence refers to a broad group of highly variable fetal malformations that are associated with fibrous bands entangling or entrapping various fetal parts in utero [1]. The most accepted pathogenic theory is the extrinsic one, in which the early partial rupture of the amniotic sac leads to the formation of fibrous bands that float in the amniotic fluid and can encircle fetal parts [2]. Due to the difficulties in diagnosing this pathology with certainty, the reported incidence varies widely, ranging from 1 in 1200 to 1 in 15,000 livebirths, and 1.8% of previable stillbirth fetuses [3, 4].
Prenatal ultrasound imaging shows thin echogenic bands attaching to both the uterine wall and associated fetal structures. The bands themselves can be difficult to detect, hence the visualization of bands is not required to suggest the diagnosis. Random anomalies that do not follow a pattern should lead the clinician to suspect amniotic band sequence and prompt close evaluation for a causative band [5, 6]. The defects resulting from the bands are categorized into various categories: neural tube-like defects, craniofacial anomalies, limb anomalies, abdominal and thoracic wall defects, and visceral anomalies [7, 8]. The most common findings are those caused by constriction rings in the limbs, which are present in at least 80% of cases. They may vary in depth, involving only the skin, to involving bone and causing edema of the distal limb, extremity asymmetry, pseudosyndactyly, or amputation of limbs or digits [8]. Histologically, constriction bands are composed of fibrous tissue containing fibroblasts covered by squamous cells, which may make them inelastic and produce a ligature effect [9]. Clubfoot deformity of the lower extremity is found in up to one third of cases, probably secondary to the presence of oligohydramnios if there is loss of amniotic fluid [6].
Cases of amniotic band sequence manifesting as constriction rings in the trunk (thorax, abdomen, or pelvis) are exceedingly rare. They were first described as abdominal constriction syndrome by Browne in 1957 [9]. The consensus is that the cause of this finding is the presence of amniotic bands, although Lin et al [10] described a case they attribute to compression by the umbilical cord. To the best of our knowledge, constriction rings in the trunk have only been described prenatally on two occasions [11,12]. The diagnosis is usually made in the newborn after birth, although most of the published cases are patients treated during childhood. To unify terminology, Graham et al [11] propose defining thoracic constriction bands as those located between the clavicles and transpyloric plane, which passes through the vertebral body of L1. Abdominal constriction bands are located between the transpyloric and intertubercular planes (through the body of L5 and iliac tubercles), and pelvic constriction bands between the intertubercular plane and ischial tuberosities. As in the extremities, these bands occur at various depths, most commonly only to the fascial layer, but they can extend down to the external or internal oblique muscles [6]. Despite the “hourglass” appearance, abdominal bands do not seem to cause mechanical problems. In mild cases the ring may become less noticeable as the child grows, therefore most authors wait until the child is about a year of age before performing surgical correction [6]. This is typically performed with excision of fibrotic tissue and Z- or W-plasties to improve appearance and to allow expansion of abdominal contents [13, 14]. Prenatally, in cases where blood flow to the cord or a limb is compromised by amniotic bands, fetal surgery may be possible. The traditional open hysterotomy approach has been progressively replaced by fetoscopic methods, which reduce complications and the need to perform a cesarean section at the time of delivery. Prenatal treatment reduces scarring compared to procedures performed after birth, due to improved dermal remodeling in the maternal uterine environment [15, 16].
Differential diagnosis includes other conditions that produce intrauterine linear echogenicities in the gravid uterus: uterine synechiae with amniotic sheets, uterine duplication anomalies, chorioamniotic nonfusion or separation, and circumvallate placenta [17]. Unlike amniotic bands, synechiae may have blood flow detected with Doppler, do not restrict fetal movements and are not associated with fetal abnormalities.
References
[1] Seeds JW, Cefalo RC, Herbert WN. Amniotic band syndrome. Am J Obstet Gynecol. 1982 Oct 1;144(3):243-8.
[2] Torpin R. Amniochorionic mesoblastic fibrous rings and amniotic bands: associated constricting fetal malformations or fetal death. Am J Obstet Gynecol. 1965 Jan 1;91:65-75.
[3] Garza A, Cordero JF, Mulinare J. Epidemiology of the early amnion rupture spectrum of defects. Am J Dis Child. 1988 May;142(5):541-4.
[4] Kalousek DK, Bamforth S. Amnion rupture sequence in previable fetuses. Am J Med Genet. 1988 Sep;31(1):63-73.
[5] Society for Maternal-Fetal Medicine; Gandhi M, Rac MWF, McKinney J. Amniotic Band Sequence. Am J Obstet Gynecol. 2019 Dec;221(6):B5-B6.
[6] Inglesby DC, Janssen PL, Graziano FD, Gopman JM, Rutland JW, Taub PJ. Amniotic Band Syndrome: Head-to-Toe Manifestations and Clinical Management Guidelines. Plast Reconstr Surg. 2023 Aug 1;152(2):338e-346e.
[7] Iqbal CW, Derderian SC, Cheng Y, Lee H, Hirose S. Amniotic band syndrome: a single-institutional experience. Fetal Diagn Ther. 2015;37(1):1-5.
[8] Kim JB, Berry MG, Watson JS. Abdominal constriction band: A rare location for amniotic band syndrome. J Plast Reconstr Aesthet Surg. 2007;60(11):1241-3.
[9] Gargh K, Sullivan C, Laing H, Banerjee S. Congenital circumferential constriction band of the abdomen: a case report. Case Rep Med. 2009;2009:825174.
[10] Lin AE, Genest DR, Brown DL. Circumferential abdominal skin defect possibly due to umbilical cord encirclement. Teratology. 1999 Nov;60(5):258-9.
[11] Graham E, Garlick JW, Johns D. Congenital Amniotic Constriction Band of the Pelvis: First Reported Case and Proposed Classification Criterion. Plast Reconstr Surg Glob Open. 2019 Jul 25;7(7):e2336.
[12] Nassr AA, Shamshirsaz AA, Belfort MA. Circumferential amniotic band around the lower fetal abdomen associated with complete spontaneous chorioamniotic separation. Am J Obstet Gynecol. 2021 Mar;224(3):312-313.
[13] Siemers F, Wünsch L, Namdar T, von Wild T, Mailänder P. Complete circumferential congenital constriction of the trunk - operation procedures and results. Ger Med Sci. 2011;9:Doc17.
[14] Ciloglu NS, Gumus N. A rare form of congenital amniotic band syndrome: total circular abdominal constriction band. Arch Plast Surg. 2014 May;41(3):290-1.
[15] Gimenez A, Kopkin R, Chang DK, Belfort M, Reece EM. Advances in Fetal Surgery: Current and Future Relevance in Plastic Surgery. Semin Plast Surg. 2019 Aug;33(3):204-212.
[16] Minella C, Costantino B, Ruano R, Koch A, Weingertner AS, Favre R, Sananes N. Fetoscopic Release of Amniotic Band Syndrome: An Update. J Ultrasound Med. 2021 May;40(5):1039-1048.
[17] Jensen KK, Oh KY, Kennedy AM, Sohaey R. Intrauterine Linear Echogenicities in the Gravid Uterus: What Radiologists Should Know. Radiographics. 2018 Mar-Apr;38(2):642-657.
Hello world
Discussion Board
We appreciate your patience as we review all submitted answers. Check back soon to see if you were correct!