Case of the Week #565
Centro Médico Recoletas, Valladolid, Spain
Case Report: A primigravida with no significant medical history presents at 20 weeks, 4 days for a second trimester examination. She reported occasional inability to urinate that resolved spontaneously. The first trimester ultrasound was normal. Transabdominal ultrasound revealed the following findings:




View the Answer Hide the Answer
Answer
We present the case of an incarcerated gravid uterus. Vaginal ultrasound examination did not identify the cervix in its usual location, as it was anteriorly displaced in the vagina. Transabdominal ultrasound demonstrated the abnormal position of an elongated cervix (72.4 mm) relative to the uterine body, which was markedly retroflexed suggesting incarceration. The uterine fundus, turned backwards within the pelvis, was situated at a lower level than the external cervical os (Image 1).
A subsequent ultrasound examination performed at 28 weeks gestation, showed a retroflexed uterus, without uterine incarceration. The cervix was positioned normally and was not stretched, contrary to its previous appearance (Image 2). The infant was delivered at 39+4 weeks via cesarean section due to non-reassuring fetal status.


Discussion
The anatomic position of the uterus is defined by the angles between the axes of the vagina, cervix, and uterine body. The angle between the cervical axis and the axis of the uterine corpus is referred to as flexion. If this angle is directed anteriorly, it is defined as anteflexion, and if is directed posteriorly, it is defined as retroflexion. Moderate flexion of the pregnant uterus is typically inconsequential, but exaggerated flexion may cause complications.
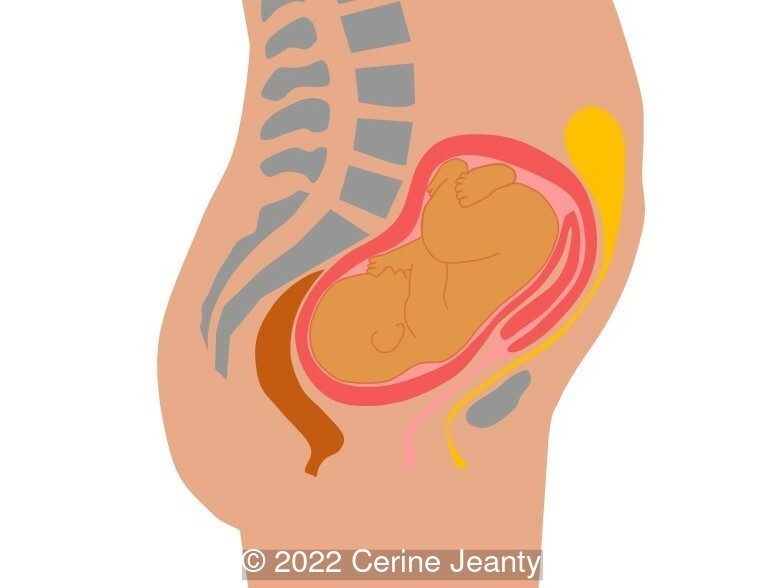
At the beginning of pregnancy, approximately 15-20% of the patients present with the uterus anatomically in retroflexion [1,2]. As gestation progresses, it spontaneously reverts anteriorly, positioning the fundus into the abdominal cavity at the end of the first trimester. In a few cases the uterus retains the retroflexed position and may become entrapped within the concavity of the sacrum between the sacral promontory and the pubic symphysis, which known as an incarcerated uterus (Image 3) [3]. As the uterus enlarges, the lower uterine segment and anterior uterine wall thin out, causing what is classically known as sacculation [4].
Uterine incarceration is a rare pathology, with an incidence that varies between 1 in 3,000 and 1 in 10,000 pregnancies [5]. If uterine incarceration is defined as the persistence of a retroflexed uterus after 16 weeks, its incidence is higher (1 in 500). Approximately 78% of cases resolve spontaneously [6]. The diagnosis should be reserved for symptomatic cases, as asymptomatic cases may be a variation of normal anatomy [6]. The first case was described in 1771 by William Hunter [7]. Although many predisposing factors for uterine incarceration have been reported, there are multiple publications describing isolated events. Known predisposing factors include uterine retroversion prior to pregnancy, previous abdominal or pelvic surgery, pelvic or uterine adhesions, leiomyomas, endometriosis, multifetal gestation, uterine anomalies, uterine prolapse, and uterine incarceration in a prior pregnancy [3,8-12].
The compression of surrounding structures by the enlarging, incarcerated uterus causes a wide variety of symptoms [13] which may include:
- Functional urinary symptoms: dysuria, urgency, cystitis, sensation of incomplete emptying, urinary retention, and overflow incontinence [14-16]
- Digestive symptoms: constipation, rectal pressure, and tenesmus [2,17]
- Pain: abdominal, suprapubic or lumbar [8,18].
Regarding obstetric complications, there can be vascular compromise that increases the risk of metrorrhagia, pregnancy loss and fetal growth restriction [3]. In contrast, there are case reports of uterine incarceration remaining asymptomatic throughout pregnancy and only diagnosed at delivery [9,19,20]. Other cases may spontaneously resolve within one to two weeks with continued growth of the uterus.
Diagnosis of this pathology may be suggested on physical examination. The cervix will be difficult to palpate and visualize on speculum examination. There may be a palpable mass in the posterior cul-de-sac, and the fundal height is less than expected for gestational age [3]. Imaging techniques to help make this challenging diagnosis include ultrasound and magnetic resonance imaging. Ultrasound may be limited as the elongated cervix can be difficult to visualize behind the pubic symphysis. Additional ultrasonographic findings include thinning of the anterior uterine wall, while there is usually thickening of the posterior wall. The bladder may appear elongated and displaced upwards. Magnetic resonance imaging can more clearly identify these findings, as well as being helpful in accurately assessing the placental location [21-23].
Initial measures to correct uterine incarceration include a knee-chest position assumed by the patient several times daily [24]. Urinary retention can be treated with an indwelling urinary catheter or intermittent self-catheterization. Persistent cases require manual repositioning, which should be performed before 20 weeks' gestation as the success rate is higher earlier in pregnancy [2, 3]. Manual reduction may cause serious complications, thus some authors consider that intervention should be reserved for symptomatic cases, and expectant management should be the standard of care [6]. Different approaches have been proposed to correct the position of the uterus [2, 3, 25]. If postural measures fail, the next option is manual reduction [12, 26-30]. After bladder catheterization, the uterus can usually be pushed out of the pelvis with the woman placed in different positions (dorsal lithotomy, Trendelenburg, lateral, all-fours, or knee-chest positions). Often, this is best accomplished by digital pressure applied through the rectum or vagina. Regional or general anesthesia can be used for patients who cannot tolerate these maneuvers. After successful reduction, patients are advised to help maintain a normal uterine position by sleeping in the prone position and by insertion of a soft pessary for a few weeks. If these maneuvers fail, reduction via colonoscopy-assisted insufflation [31, 32] and upward round ligament traction during laparoscopy or laparotomy has been described [25].
If reduction of the incarcerated gravid uterus is not possible, cesarean delivery is the recommended route of delivery [2, 3]. In this case, the anatomic changes that occur in the position of the uterine segment, the bladder, and the cervix must be considered to avoid excessive blood loss and possible injuries during surgery [19, 33].
References
[1] Feusner AH, Mueller PD. Incarceration of a gravid fibroid uterus. Ann Emerg Med. 1997 Dec;30(6):821-4. doi: 10.1016/s0196-0644(97)70058-1. PMID: 9398784.
[2] Jacobsson B, Wide-Swensson D. Incarceration of the retroverted gravid uterus--a review. Acta Obstet Gynecol Scand. 1999 Sep;78(8):665-8. PMID: 10468056.
[3] Shnaekel KL, Wendel MP, Rabie NZ, et al. Incarceration of the Gravid Uterus. Obstet Gynecol Surv. 2016 Oct;71(10):613-619. PMID: 27770131.
[4] Spearing GJ. Uterine sacculation. Obstet Gynecol. 1978 Jan;51(1 Suppl):11s-13s. PMID: 618466.
[5] van Beekhuizen HJ, Bodewes HW, Tepe EM, et al. Role of magnetic resonance imaging in the diagnosis of incarceration of the gravid uterus. Obstet Gynecol. 2003 Nov;102(5 Pt 2):1134-7. PMID: 14607032.
[6] Tachibana D, Misugi T, Kitada K, K et al. Incarcerated Gravid Uterus: Spontaneous Resolution Is Not Rare. Diagnostics (Basel). 2021 Aug 25;11(9):1544. PMID: 34573886
[7] Longo LD. Classic pages in obstetrics and gynecology. On retroversion of the uterus. William Hunter. Medical Observations and Inquiries, vol. 4, pp. 400-409, 1771. Am J Obstet Gynecol. 1978 May 1;131(1):95-6. PMID: 347937.
[8] Sweigart AN, Matteucci MJ. Fever, sacral pain, and pregnancy: an incarcerated uterus. West J Emerg Med. 2008 Nov;9(4):232-4. PMID: 19561753
[9] Dierickx I, Mesens T, Van Holsbeke C, et al. Recurrent incarceration and/or sacculation of the gravid uterus: a review. J Matern Fetal Neonatal Med. 2010 Aug;23(8):776-80. PMID: 19903108.
[10] Al Wadi K, Helewa M, Sabeski L. Asymptomatic uterine incarceration at term: a rare complication of pregnancy. J Obstet Gynaecol Can. 2011 Jul;33(7):729-732. PMID: 21749750.
[11] Katopodis C, Menticoglou S, Logan A. Incarcerated fibroid uterus: the role of conservative management. J Obstet Gynaecol Can. 2013 Jun;35(6):536-538. PMID: 23870778.
[12] Kim HS, Park JE, Kim SY, et al. Incarceration of early gravid uterus with adenomyosis and myoma: report of two patients managed with uterine reduction. Obstet Gynecol Sci. 2018 Sep;61(5):621-625. PMID: 30254999
[13] Han C, Wang C, Han L, et al. Incarceration of the gravid uterus: a case report and literature review. BMC Pregnancy Childbirth. 2019 Nov 8;19(1):408. PMID: 31703641
[14] Love JN, Howell JM. Urinary retention resulting from incarceration of a retroverted, gravid uterus. J Emerg Med. 2000 Nov;19(4):351-4. PMID: 11074329.
[15] Yang JM, Huang WC. Sonographic findings in acute urinary retention secondary to retroverted gravid uterus: pathophysiology and preventive measures. Ultrasound Obstet Gynecol. 2004 May;23(5):490-5. PMID: 15133802.
[16] Slama R, Barry M, McManus K, et al. Uterine Incarceration: Rare Cause of Urinary Retention in Healthy Pregnant Patients. West J Emerg Med. 2015 Sep;16(5):790-2. PMID: 26587114
[17] Lettieri L, Rodis JF, McLean DA, et al. Incarceration of the gravid uterus. Obstet Gynecol Surv. 1994 Sep;49(9):642-6. PMID: 7991232.
[18] Frei KA, Duwe DG, Bonel HM, et al. Posterior sacculation of the uterus in a patient presenting with flank pain at 29 weeks of gestation. Obstet Gynecol. 2005 Mar;105(3):639-41. doi: 10.1097/01.AOG.0000141695.83741.94. PMID: 15738037.
[19] van der Tuuk K, Krenning RA, Krenning G, et al. Recurrent incarceration of the retroverted gravid uterus at term - two times transvaginal caesarean section: a case report. J Med Case Rep. 2009 Nov 3;3:103. PMID: 19946581
[20] Hsu PC, Yu MH, Wang CY, et al. Asymptomatic uterine incarceration at term: Successful management of a rare complication in pregnancy. Taiwan J Obstet Gynecol. 2018 Oct;57(5):745-749. PMID: 30342664.
[21] Gottschalk EM, Siedentopf JP, Schoenborn I, et al. Prenatal sonographic and MRI findings in a pregnancy complicated by uterine sacculation: case report and review of the literature. Ultrasound Obstet Gynecol. 2008 Sep;32(4):582-6. PMID: 18677703.
[22] Fernandes DD, Sadow CA, Economy KE, et al. Sonographic and magnetic resonance imaging findings in uterine incarceration. J Ultrasound Med. 2012 Apr;31(4):645-50. PMID: 22441922.
[23] Gardner CS, Jaffe TA, Hertzberg BS, et al. The incarcerated uterus: a review of MRI and ultrasound imaging appearances. AJR Am J Roentgenol. 2013 Jul;201(1):223-9.PMID: 23789679.
[24] Cunningham FG, Leveno KJ, Dashe JS, H et al. Congenital Genitourinary Abnormalities. In: Williams Obstetrics, 26e, McGraw Hill, New York, 2022; pages 31-50.
[25] Kim YS, Kwon BS, Lee YJ. Clinical approach and management of uterine incarceration according to trimester of pregnancy: Case report and literature review. Taiwan J Obstet Gynecol. 2021 Sep;60(5):911-915. PMID: 34507673.
[26] Inaba F, Kawatu T, Masaoka K, et al. Incarceration of the retroverted gravid uterus: the key to successful treatment. Arch Gynecol Obstet. 2005 Nov;273(1):55-7. PMID: 15551143.
[27] Grossenburg NJ, Delaney AA, Berg TG. Treatment of a late second-trimester incarcerated uterus using ultrasound-guided manual reduction. Obstet Gynecol. 2011 Aug;118(2 Pt 2):436-439. doi: 10.1097/AOG.0b013e3182164864. Erratum in: Obstet Gynecol. 2011 Dec;118(6):1424. PMID: 21768846.
[28] Policiano C, Araújo C, Santo S, et al. Incarcerated gravid uterus: early manual reduction vs. late spontaneous resolution. Eur J Obstet Gynecol Reprod Biol. 2014 Sep;180:201-2. PMID: 24910317.
[29] Gardner B, Kozakiewicz ML, Whitecar PW, et al. Novel Approach to Reduction of an Incarcerated Uterus. Obstet Gynecol. 2018 Nov;132(5):1177-1179. PMID: 30303919.
[30] Suzuki S, Obata S, Utsunomiya M, M et al. A case of incarcerated gravid uterus with a history of cesarean section was a good candidate for manual reduction: A case report. Clin Case Rep. 2020 Nov 12;9(1):322-325. PMID: 33489179; PMCID: PMC7813024.
[31] Seubert DE, Puder KS, Goldmeier P, et al. Colonoscopic release of the incarcerated gravid uterus. Obstet Gynecol. 1999 Nov;94(5 Pt 1):792-4. PMID: 10546731.
[32] Dierickx I, Van Holsbeke C, Mesens T, et al. Colonoscopy-assisted reposition of the incarcerated uterus in mid-pregnancy: a report of four cases and a literature review. Eur J Obstet Gynecol Reprod Biol. 2011 Oct;158(2):153-8. PMID: 21741751.
[33] Samejima K, Matsunaga S, Takai Y, et al. Efficacy of well-planned management in patients with incarcerated gravid uterus: A case series and literature review. Taiwan J Obstet Gynecol. 2021 Jul;60(4):679-684. PMID: 34247806.
Discussion Board
Winners

Dianna Heidinger United States Sonographer

Umber Agarwal United Kingdom Maternal Fetal Medicine

Ana Ferrero Spain Physician

Mayank Chowdhury India Physician

Daniel Kato Brazil Physician

Vladimir Lemaire United States Physician

Nguyen Luân Viet Nam Physician
ALBANA CEREKJA Italy Physician

Murat Cagan Turkey Physician

Karin Tinnemeier Germany Physician

Daniil Gagaev Russian Federation Physician

liesbeth lewi Belgium Physician

Kathy Hasiak United States Sonographer