Case of the Week #622
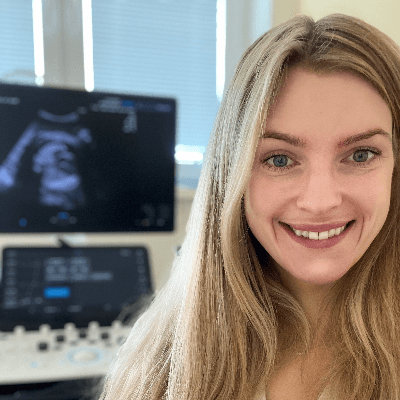
(1) Department of Genetics, (2) Department of Fetal Cardiology, Polish Mother's Memorial Hospital, Lodz, Poland; (3) Hospital Recoletas Campo Grande, Valladolid, Spain
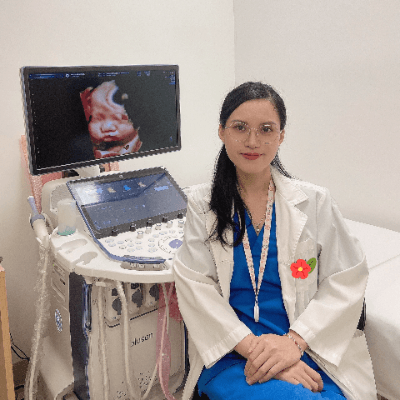
36-year-old primigravida with no past medical history was referred due to a suspicion of fetal posterior fossa anomaly at 21 weeks, 6 days. The following images were obtained. The remainder of the exam was normal.
View the Answer Hide the Answer
Answer
We present a case of Torcular Herophili Thrombosis with favorable outcome. No maternal or placental abnormalities were identified, and the thrombus was an isolated event.
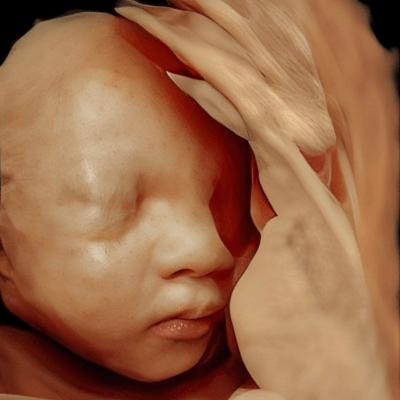
Our ultrasound demonstrated a singleton live fetus with normal movement and muscle tone. Amniotic Fluid Index was slightly elevated at 20 cm. There was enlargement of the torcular Herophili with a central thrombus causing mass effect and inferior displacement of the cerebellum, compression and displacement of lateral ventricles, as well as flattening of the cisterna magna. Additionally, the mass effect caused distortion of other structures, including the corpus callosum. Collateral circulation within scalp could be seen (Video 3). Other brain structures, including thalami, falx cerebri, and midbrain, appeared normal.
The patient was monitored closely. MRI was not performed because the patient resided far from tertiary care centers, and the risk of preterm labor precluded long-distance travel. Over the course of the pregnancy, the thrombotic mass gradually diminished, resolving completely by term. The patient delivered an apparently healthy newborn. Postnatal brain imaging (ultrasound and MRI) showed no abnormalities. At three years of age, the child’s development was assessed as normal.
Discussion
Cerebral vascular malformations are rare but potentially disastrous abnormalities. Aneurysm of the vein of Galen is the most common abnormality described in prenatal series. Other intracranial vascular malformations diagnosed prenatally include venous anomalies, such as dural sinus malformations, and arterial anomalies, such as pial arteriovenous fistulas [1].
The dural venous sinuses are a drainage system that regulates blood flow from the superficial and deep cerebral veins, meninges, and calvarium to the internal jugular veins at the base of the skull. They are endothelium-lined intracranial channels characterized by the lack of muscular walls and venous valves. There are seven major dural venous sinuses located within the cranial cavity between the periosteal and meningeal layer of the dura mater, including the superior sagittal, inferior sagittal, straight, transverse, sigmoid, cavernous, and superior petrosal sinuses [2]. The term torcular Herophili (or torcula) takes the name of Herophilus of Alexandria (325-255 BC), Father of Anatomy, indicating the “confluence of sinuses,” which is the intersection of the superior sagittal and straight sinuses with the two transverse sinuses located at the junction of the tentorium cerebelli and the falx cerebri [3].
Torcular Herophili thrombosis is a rare but significant finding during prenatal imaging, characterized by thrombus formation in the confluence of venous sinuses at the base of the fetal brain. Most reported cases are associated with a dural sinus malformation that presents with a dilated dural sinus pouch communicating with the other sinuses and draining cerebral veins [4]. The possibility of a venous thrombosis without underlying dural sinus malformation is unlikely, although it has been reported in the absence of a dural sinus malformation and in locations other than the torcula [5].
Several hypotheses have been proposed to explain the genesis of a dural sinus malformation. It could be due to the persistence of physiologic ballooning of the transverse or posterior portion of the superior sagittal sinus between the fourth and sixth month of fetal development [6, 7], or be the consequence of an excessive and anarchic sinus development [4]. In either case, the appearance of thrombosis represents a secondary, non-causal phenomenon as is demonstrated in a case reported by Grange et al. The group images a fetus with a patent dural sinus malformation that is complicated by thrombosis on subsequent imaging during pregnancy [8]. The thrombosis might be secondary to accessory low-flow shunts of the walls of the sinus, immaturity of the sinus, or modification of the endothelial walls [9].
The etiology of prenatal venous sinus thrombosis remains unclear in most cases but may involve a combination of maternal, fetal, and placental factors. Vascular anatomic malformations affecting the drainage into the torcular herophili is the most common condition associated with these cases [10]. Hypercoagulable states, infections, polycythemia, trauma or structural abnormalities in the fetal venous system have been implicated postnatally [11].
High resolution prenatal ultrasound and fetal MR imaging are essentials tools in diagnosing and monitoring torcular Herophili thrombosis. A key feature on ultrasound is the detection of a hyperechogenic round mass, representing a blood clot, attached to the wall of a dilated torcular Herophili above the tentorium, in the confluence of sinuses [10]. The dilatation of the torcula, grossly triangular-shaped, produces secondary displacement of the cerebellum, flattening of the cisterna magna and potential compression of the lateral ventricles resulting in ventriculomegaly. The presence of a small amount of cerebrospinal fluid between the mass and the vermis easily identifies the mass within the dura [4]. On color Doppler imaging, there is no flow inside the mass due to low flow velocity and/or the presence of thrombus. However, there may be vascularity at the margin of the lesion, which might represent the multiple mural arteriovenous shunts [12]. The velocity of these shunts is usually low, and they rarely cause systemic hemodynamic complications [13]. On MR imaging analysis, the dural sinus malformation appears as a well-circumscribed mass with a heterogeneous hypointense signal on T2-weighted images and a hyperintense signal in T1-weighted images due to clotted blood [4].
This condition poses potential risks due to its mass effect on surrounding structures and the possibility of associated complications, such as increased intracranial pressure, hydrocephalus and ischemic brain damage [9]. Venous hypertension could result in a failure of cerebrospinal fluid resorption through the venous system leading to hydrocephalus and brain infarction or hemorrhage [4]. However, when Torcular Herophili thrombosis is isolated and diagnosed early, the prognosis can be favorable in 62-70% of cases with gradual resolution of the mass and good long-term neurological outcomes [14-17]. Resolution of the thrombosis is thought to occur due to the presence of several anastomoses between the superficial and deep venous territories in fetal life without substantial impairment of cerebral circulation. Possible indicators of good prognosis include decrease in size of the mass, as well as clot formation and even clot enlargement which may suggest involution of dural sinus malformation [18,19]. The normal neurodevelopmental outcome in this case underscores the importance of distinguishing isolated cases from those with additional risk factors or abnormalities.
Although several authors have recommended expectant management throughout pregnancy with serial imaging to assess changes in the thrombus size, and any progression of mass effect or ventriculomegaly [20-23], pregnancy termination rates remain as high as 26% [24]. Vaginal delivery does not seem to be contraindicated in cases with spontaneous regression of the dural sinus thrombosis. However, if instrumental extraction is necessary, vacuum extraction should probably be avoided, as its use may be associated with cephalohematomas [21]. Delivery planning may require coordination with a multidisciplinary team if complications are anticipated. Postnatal imaging, including brain ultrasound and MRI, is recommended to evaluate resolution and exclude residual abnormalities.
Differential diagnosis include other fluid collections located in the posterior fossa including retrocerebellar arachnoid cysts, subdural or large intraparenchymal hematomas, Dandy–Walker malformation, megacisterna magna, and vascular malformations such as the aneurysm of the Vein of Galen. Other considerations include rare instances of congenital tumors, especially teratomas [12].
Prenatal torcular Herophili thrombosis, while rare, highlights the value of advanced imaging and multidisciplinary care in optimizing outcomes. Early diagnosis and monitoring are critical in identifying cases with favorable prognoses, allowing for appropriate counseling and management.
References
[1] Bhide A. Vascular Cerebral Anomalies. In: Copel JA, ed. Obstetric Imaging. Fetal Diagnosis and Care, 2nd ed. Elsevier, Philadelphia, PA, USA, 2018; pag 226-230.e1.
[2] Bayot ML, Reddy V, Zabel MK. Neuroanatomy, Dural Venous Sinuses. [Updated 2023 Aug 8]. In: StatPearls [Internet]. Treasure Island (FL): StatPearls Publishing; 2025 Jan-. Available from: https://www.ncbi.nlm.nih.gov/books/NBK482257/
[3] McCormack IG, Neumann PE, Tubbs RS. Torcular Herophili: A Review of the History of the Term and Synonyms. World Neurosurg. 2022 Mar; 159:120-125.
[4] Merzoug V, Flunker S, Drissi C, et al. Dural sinus malformation (DSM) in fetuses. Diagnostic value of prenatal MRI and follow-up. Eur Radiol. 2008 Apr; 18(4):692-9.
[5] Lacalm A, Garel C, Massoud M, et al. Prenatal diagnosis of multiple cortical and deep cerebral vein thromboses in the absence of dural venous malformation. Ultrasound Obstet Gynecol. 2015 Apr; 45(4):486-8.
[6] Okudera T, Huang YP, Ohta T, et al. Development of posterior fossa dural sinuses, emissary veins, and jugular bulb: morphological and radiologic study. AJNR Am J Neuroradiol. 1994 Nov; 15(10):1871-83.
[7] McInnes M, Fong K, Grin A, et al. Malformations of the fetal dural sinuses. Can J Neurol Sci. 2009 Jan; 36(1):72-7.
[8] Grangé G, LeTohic A, Merzoug V, Adamsbaum C. Prenatal demonstration of afferent vessels and progressive thrombosis in a torcular malformation. Prenat Diagn. 2007 Jul; 27(7):670-3.
[9] Byrd SE, Abramowicz JS, Kent P, et al. Fetal MR imaging of posterior intracranial dural sinus thrombosis: a report of three cases with variable outcomes. Pediatr Radiol. 2012 May; 42(5):536-43.
[10] Corral E, Stecher X, Malinger G, et al. Thrombosis of the torcular herophili in the fetus: a series of eight cases. Prenat Diagn. 2014 Dec; 34(12):1176-81.
[11] Stam J. Thrombosis of the cerebral veins and sinuses. N Engl J Med. 2005 Apr 28; 352(17):1791-8.
[12] Rossi A, De Biasio P, Scarso E, et al. Prenatal MR imaging of dural sinus malformation: a case report. Prenat Diagn. 2006 Jan; 26(1):11-6.
[13] Pandey V, Dummula K, Parimi P. Antenatal thrombosis of torcular herophili presenting with anemia, consumption coagulopathy and high-output cardiac failure in a preterm infant. J Perinatol. 2012 Sep; 32(9):728-30.
[14] Karl K, Heling KS, Chaoui R. Ultrasound of the Fetal Veins Part 3: The Fetal Intracerebral Venous System. Ultraschall Med. 2016 Feb; 37(1):6-26.
[15] Gicquel JM, Potier A, Sitruk S, Girard N. Normal outcome after prenatal diagnosis of thrombosis of the torcular Herophili. Prenat Diagn. 2000 Oct; 20(10):824-7.
[16] Jung E, Won HS, Kim SK, et al. Spontaneous resolution of prenatally diagnosed dural sinus thrombosis: a case report. Ultrasound Obstet Gynecol. 2006 May; 27(5):562-5.
[17] Simsek Y, Oztanir N, Sigirci A, et al. Spontaneous resolution of fetal dural sinus thrombosis following term delivery of a live infant. Ultrasound Obstet Gynecol. 2012 Nov; 40(5):614-5.
[18] Laurichesse Delmas H, Winer N, et al. Prenatal diagnosis of thrombosis of the dural sinuses: report of six cases, review of the literature and suggested management. Ultrasound Obstet Gynecol. 2008 Aug; 32(2):188-98.
[19] Yang E, Storey A, Olson HE, et al. Imaging features and prognostic factors in fetal and postnatal torcular dural sinus malformations, part II: synthesis of the literature and patient management. J Neurointerv Surg. 2018 May; 10(5):471-475.
[20] Grigoriadis S, Cohen JE, Gomori JM. Prenatal thrombosis of torcular Herophili with spontaneous resolution and normal outcome. J Neuroimaging. 2008 Apr; 18(2):177-9.
[21] Legendre G, Picone O, Levaillant JM, et al. Prenatal diagnosis of a spontaneous dural sinus thrombosis. Prenat Diagn. 2009 Aug; 29(8):808-13.
[22] Fanou EM, Reeves MJ, Howe DT, et al. In utero magnetic resonance imaging for diagnosis of dural venous sinus ectasia with thrombosis in the fetus. Pediatr Radiol. 2013 Dec; 43(12):1591-8.
[23] Has R, Esmer AC, Kalelioglu I, et al. Prenatal diagnosis of torcular herophili thrombosis: report of 2 cases and review of the literature. J Ultrasound Med. 2013 Dec; 32(12):2205-11.
[24] Sacco A, Pannu D, Ushakov F, et al. Fetal dural sinus thrombosis: A systematic review. Prenat Diagn. 2021 Jan; 41(2):248-257.
Discussion Board
Winners

Irina Morozova Russian Federation Physician

Dianna Heidinger United States Sonographer

Yulia Sologub Russian Federation Physician

Javier Cortejoso Spain Physician
paola quaresima Italy Physician

Igor Yarchuk United States Sonographer

Andrii Averianov Ukraine Physician

Ana Ferrero Spain Physician

Alexandr Krasnov Ukraine Physician

Mayank Chowdhury India Physician
Adrian Popa Romania Physician

Vladimir Lemaire United States Physician
Ivan Ivanov Russian Federation Physician
Boujemaa Oueslati Tunisia Physician

Tatiana Koipish Belarus Physician

PRIYA R United States Physician

Peter conner Sweden Physician

Panagiotis Benardis Greece Physician

Kimberly Delaney United States Sonographer

Olivia Ionescu United Kingdom Physician
Marianovella Narcisi Italy Physician
Rebecca Evans Australia Sonographer

CHEN YANG China Sonographer

Elena Andreeva Russian Federation Physician

Muradiye Yıldırım Turkey Physician

CRISTINA MARTINEZ PAYO Spain Physician
ALBANA CEREKJA Italy Physician

Yana Semina Russian Federation Physician
Eti Zetounie Israel Sonographer

Deval Shah India Physician

ALPESH PANCHOLI United States

Sonio Sonio France AI
ANA PAULA PASSOS Brazil Physician

Büşra Cambaztepe Turkey Physician

Ionut Valcea Romania Physician
Đặng Mai Quỳnh Viet Nam Physician

Almaz Kinzyabulatov Russian Federation Physician

Kareem Haloub Australia Physician

Dr Monika Sharma India Physician
Anette Beverdam Netherlands Sonographer
Fred Pop Uganda Sonographer

Annette Reuss Germany Physician

Vandana Yakub India Physician

Arati Appinabhavi India Physician
shruti Agarwal India Physician
shay kevorkian Israel Physician

Kedarnath Dixit India Physician
Mahmoud Moussa United Kingdom Physician

Kim Sochetra Cambodia Sonographer
Sruthi Pydi India Physician
Azam Malek Ghasemi United Arab Emirates Physician

Rupal Sasani India Physician
Eylem Eşsizoğlu Turkey Physician

Denys Saitarly Israel Physician

Tetiana Ishchenko Ukraine Physician
Le Duc Viet Nam Physician
Zuzana Rak Slovakia Physician

Hana Habanova Slovakia Physician
Tamara Yarygina Russian Federation Physician

Stefan Schmitt- Heidsieck Germany Physician

Islam El Gezeiry Egypt Physician

Robert Brawura-Biskupski-Samaha Poland Physician

Viktoriia Putsenko Russian Federation Physician

FIRAT ERSAN Turkey Physician

Ali Ozgur Ersoy Turkey Physician

ZHANNA Kurmangaliyeva Kazakhstan Врач ультразвуковой диагностики

Liam McCullough Slovakia Physician

Yuliya Ursu United Kingdom Physician

Natalia Omelyanovich Russian Federation Physician

Murad Esetov Russian Federation Physician